Tahira Khan
Khalida Bibi* is a resident of Killi Toor Kuch, Hanna Urak, who lost her infant baby last week. According to doctors, her baby got an infection during the delivery process and did not survive for more than five days. It is pertinent to note that Killi Toor Kuch does not have Primary Healthcare (PHC) facilities to help with neonatal care of newborns.
In such spirit, neonatal care is required when the baby is born either sick or premature. Therefore, in such conditions, the baby is placed in an Intensive Care Unit in the hospital that provides basic health facilities. Basically, neonatal means “newborn” and covers the first month after birth. In the same vein, the post-natal period covers the remaining eleven-month period.
Following that, Killi Toor Kuch is a village at Hanna Urak that is approximately 21 kilometers away from the main Quetta city. In 2022, flash flooding swept away critical infrastructure such as roads and bridges in the village. It also damaged houses, schools, healthcare facilities, and livestock due to which many households have migrated from the village. Regrettably, Khalida Bibi belongs to one of those households that could not migrate to other urban centers. She lives with a family of six in a shelter provided by the NGOs.
In addition to that, there is currently one MNCH (Maternal, Newborn, and Child Health) Centre working at Hanna Urak whereas roads leading to the center from different villages are damaged severely. Additionally, Journalist Asim Ahmed Khan said that last year’s flood also destroyed one of the BHU (Basic Health Unit) of Hanna Urak which has further hampered the provision of healthcare facilities.
In her words;
“When I delivered a baby I was overwhelmed with emotions and excitement but that did not last long. I could not find words to describe the agony I felt when my baby stopped breathing. My husband rushed to MNCH Quetta but that did not bring any good news.”
The tale of Khalida Bibi is not new in Balochistan. Neo-natal deaths are linked mostly to maternal care taken during the pregnancy period. A report titled “Predictors and disparities n neo-natal and under 5 mortality in rural Pakistan: a cross-sectional analysis”, 2023, mentioned that the absence of obstetric care during delivery and lack of managing preterm birth complications lead to high neo-natal mortality rates in rural areas. However, in the context of post-natal care vaccinations, nutrition, sanitation, and access to clean water play a vital role.
In a research report titled “Time to Focus Child Survival Programs on the Newborn: Assessment of Levels and Causes of Infant Mortality in Rural Pakistan”, 2002, it is revealed that unhygienic practices during delivery are adopted in various cities of Balochistan including Quetta and the associated villages. These practices include application of ghee to the umbilical cord and raping neonate in sheepskin. Further, Dr. Maria Ali Khan also confirmed that many neonate deaths occur due to these unhygienic practices and lack of vaccination process.
As per the United Nations Children’s Fund (UNICEF) report, 2023, it is ten times more probable in underdeveloped areas that a baby would die in the first month than in any other developed region. As far as Balochistan is concerned, it has the highest score of neonatal deaths i.e., 63 deaths per thousand live births. Globally, Pakistan ranks third most risk country in the context of neonatal mortality rate.
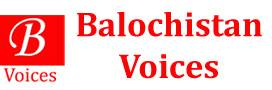
Accordingly, every year the country encounters two lakh ninety-eight thousand neonatal deaths with a neonatal mortality rate (NMR) constituting 42 deaths per thousand live births. Briefly, the country is responsible for seven percent of neonatal deaths around the globe. In the context of the South Asian region, the Estimate generated by the UN inter-agency Group for Child Mortality Estimation (UN IGME), 2023, did not picture a positive image of Pakistan as compared to India and Afghanistan. Pakistan lags behind India and other South Asian countries in lowering the child mortality rate as shown below;
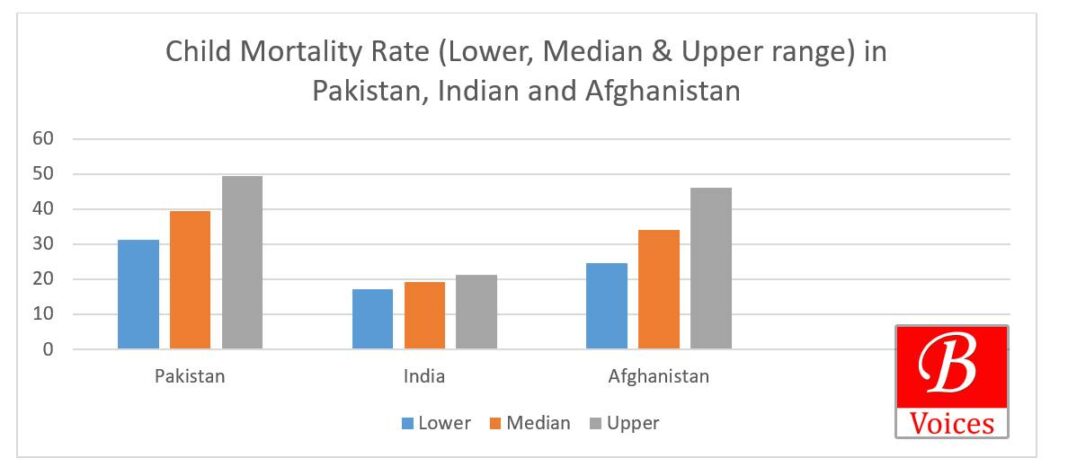
As far as Pakistan is concerned, researchers have also witnessed marked disparities that exist with regard to child mortality within provinces and regions i.e., urban and rural. At the provincial level, Balochistan has a bleak picture due to its poverty index and lack of awareness along with critical health infrastructure. Despite having a lower population ratio as compared to other provinces, its score is high in the context of neonatal mortality rate with Jafferabad with the highest NMR i.e., 87 deaths per 1000 live births.
Following that, Dr. Maria Ali Khan stated that Neonatologists best deal with newborns, and currently there are only a few Neonatologists in Balochistan. Similarly, Dr. Faryal Khan, LMO at Kacchi District, commented on the reasons behind the precarious health sector of the province. According to her, the health sector has birth centers but they could not cover the sparsely populated population of Balochistan. Besides, she also lamented the fact the province does not have enough skilled birth attendants or LHVs for far-flung areas where gynecologists cannot reach at the time of delivery.
Moreover, she commented that even in Quetta there is a dearth of well-equipped intensive Care Units for newborns let alone Killi Toor Kuch or Killi Abdul Wahid Kakar which lies in the suburbs of Quetta city. As per the government strategy to deal with the neo-natal mortality rate, it is recommended that one trained LHV should be posted in one pocket of the population even if the pocket consists of four houses. However, the strategy has not been successfully implemented in the province.
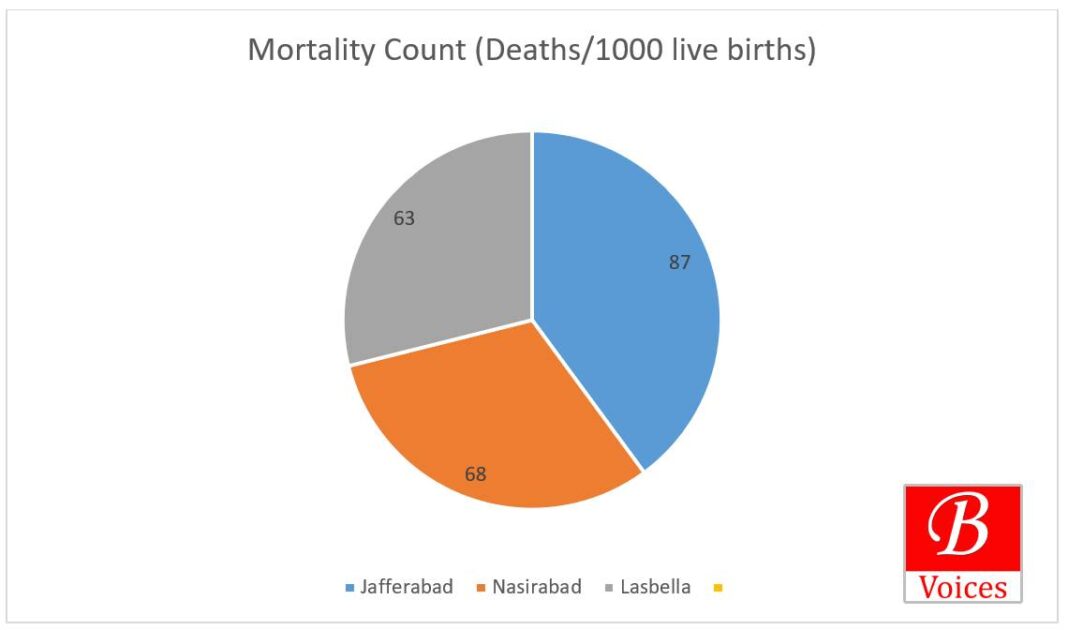
Moreover, there is a dearth of research surveys to assess the existing healthcare facilities in Balochistan. In one of the reports, it is mentioned that there are only 177 healthcare facilities in Balochistan. Among those facilities, 145 are providing Primary health care (PHC) facilities that are not enough to cover the whole province. In the context of Secondary Healthcare facilities(SHC), only 27 facilities are available for the purpose whereas only 5 units can provide Tertiary Healthcare (THC) facilities.
The report further explores that the province has only three intensive care units for newborns with a minimum level of staff. Maryum Aman, a multimedia journalist based in Quetta, also commented on the matter. According to her, many hospitals in Quetta city do not have any policy to manage the staff-patient ratio. Almost every healthcare facility is devoid of staff and trained doctors to look after neonatal complications.
Dr. Paras Shezad, Pediatrician and Neonatalogist, at Nagi Hospital, Quetta explained why the neo-natal death rate is high in Balochistan. According to him, there could be multiple reasons behind NMR but the conservative code of conduct and infections are the major reasons. Moreover, he also mentioned that it is customary practice in Balochistan where mothers avoid pre-natal and post-natal visits because of which most of the babies are born either underweight or premature.
Accordingly, he stated that it is very pertinent for any mother to provide post-natal care to newborns within 48 hours but people rely on cultural methods of healthcare not following immunization follow-ups and proper breast-feeding habits.
Similarly, to avoid infections, vaccinations play a crucial role whereas people doubt the very idea of vaccination. It is because of this, that basic vaccination coverage is least prevalent in Balochistan I.e. 29%. When asked about government initiatives, he said the recent step is the introduction of a health card scheme where families can avail of free medical facilities up to one million rupees in seventeen different hospitals in Balochistan.
The writer holds an M.Phil Degree in South Asian Studies from the University of Punjab. She can be reached on Twitter @TahiraGhilzai.
Click here to read previous articles of the writer.
Share your comments!